
Mast cells are a special type of blood cell that are normally involved in the body’s response to allergens and inflammation. When these cells mutate, they develop in to a mast cell tumor. Mast cell tumors most commonly found on the skin, but other sites can include the lymph nodes, spleen, liver, bone marrow and intestines. Mast cell tumors can look like anything, but most often are raised, red, hairless masses that can wax and wane in size. Mast cells contain substances within their granules (most common ones are histamine and heparin) that can cause the local inflammation (redness and swelling) and possible bleeding. Due to the effects of the granules, most patients will be started on anti-histamines and antacids for supportive care.
Mast cells are a special type of blood cell that are normally involved in the body’s response to allergens and inflammation. When these cells mutate, they develop in to a mast cell tumor. Mast cell tumors most commonly found on the skin, but other sites can include the lymph nodes, spleen, liver, bone marrow and intestines. Mast cell tumors can look like anything, but most often are raised, red, hairless masses that can wax and wane in size. Mast cells contain substances within their granules (most common ones are histamine and heparin) that can cause the local inflammation (redness and swelling) and possible bleeding. Due to the effects of the granules, most patients will be started on anti-histamines and antacids for supportive care.
It is recommended that any new lump or bump be evaluated by your veterinarian. There are several breeds who at a higher risk of developing mast cell tumors in their lifetime. These breeds include Boxers, Bulldogs, Pitbulls, Pugs and Boston Terriers, but dogs of any breed can be diagnosed with a mast cell tumor.

Diagnosis
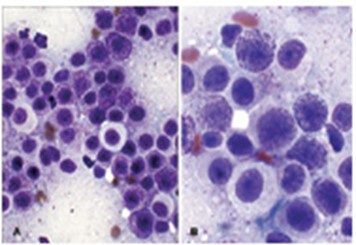
A mast cell tumor is usually diagnosed by fine needle aspiration. This procedure entails inserting a needle into the mass and aspirating back some cells. The cells that are removed are put on a slide and sent out to the laboratory for the pathologist to review.
Mast cell tumors have a varying behavior where some may be slow growing and less aggressive, while others will grow quickly and cause discomfort. Initial evaluation of a dog with a mast cell tumor usually involves additional diagnostics to determine the extent of disease (also known as staging the disease). The most common sites for metastasis are the draining lymph nodes, liver, spleen and rarely the bone marrow. Additional diagnostics include bloodwork (complete blood count and chemistry panel), urinalysis, chest radiographs, regional lymph node aspiration, abdominal ultrasound to evaluate the liver, spleen and lymph nodes and possible aspiration of the spleen and liver. Although rare, a bone marrow aspirate may also be recommended. There are additional tests that can be done to try and predict the behavior of the mast cell tumor. This can include testing for a mutation called c-kit or performing a mast cell tumor panel.
Mast cell tumors are graded in two ways:
-
Patnaik scale: Tumors are graded I-III. Grade I tumors are the least aggressive, Grade II tumors are the most common and Grade III tumors are the most aggressive and carry a worse prognosis compared to lower grades.
-
Two Tier Scale: Tumors are graded high or low. Low grade mast cell tumors are considered locally aggressive. High grade mast cell tumors are not only locally aggressive but are likely to spread to other areas of the body and carry a more guarded prognosis.
Treatment
Treatment options for cutaneous mast cell tumors may include surgery, radiation therapy, chemotherapy and/or supportive care.
The gold standard of treatment is surgery to remove the mass. Mast cell tumors can be invasive, and because of this, the surgeon will want to be aggressive by taking a large margin both around and under the tumor to try and ensure complete removal. Unfortunately, even when a large margin is taken, there is a chance that some of the tumor cells remain along the surgical site. When a mast cell tumor is not completely excised, the main concern is for recurrence along the scar. If incomplete margins are found, then options include additional surgery (if possible) or radiation therapy.
The goal of radiation is to try and clean up the residual disease that remains to slow the rate of recurrence. Fortunately, radiation is very effective at preventing/slowing local recurrence of mast cell tumors. Radiation therapy is administered while the patient is under anesthesia and consists of a daily treatment, Monday through Friday, for 3-4 weeks in a row. Studies have found local disease control times of 2-5 years for patients with grade I and II mast cell tumors who are treated with surgery and radiation.
Surgery and radiation therapy are local treatments and have no effect on the spread of the tumor. Chemotherapy is beneficial for patients with metastatic disease, when the tumor is too large for surgery, or when there is a high risk for metastasis. Chemotherapy can be used in combination with surgery or alone, but it is much more effective if the tumor has been removed.
Fortunately, chemotherapy is well tolerated by most patients. Side effects that can be seen include stomach upset, decrease in the white blood cell count and possible thinning of the fur coat. 10% of patients treated will experience significant side effects that warrant a visit to the hospital for outpatient care and 1% will experience life threatening side effects or need to be hospitalized.
Supportive medications usually include antihistamine and antacid, +/- predisione.
Prognosis
The prognosis or outcome for cutaneous mast cell tumors depends upon several factors. This includes grade of the tumor, location of the tumor, whether or not the tumor is positive for the kit mutation, and the presence of metastasis. Once a patient develops a mast cell tumor, they are at risk for developing additional ones in the future. The majority of mast cell tumors can be successfully treated when found and treated early.
The goal of any treatment option is to help maintain a good quality of life for your pet for as long as we can. Your oncologist will be able to discuss the treatment options available and what is best for your pet.
