What is Myasthenia Gravis?
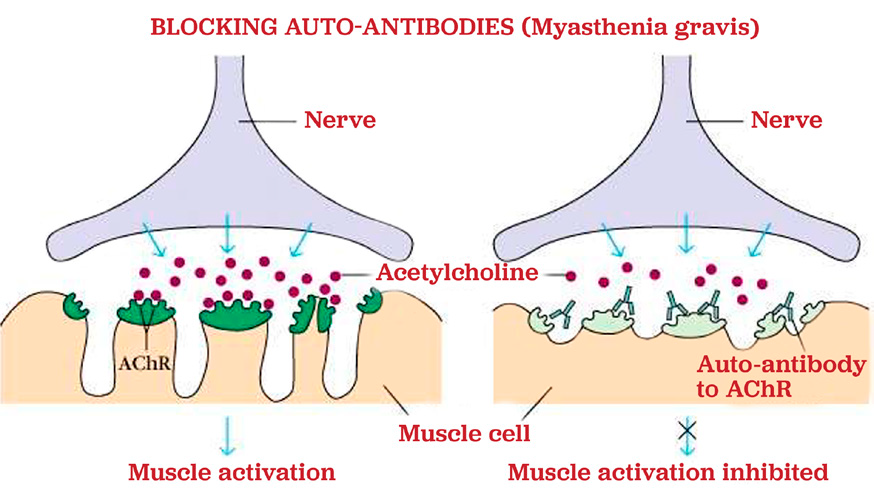
In order for muscles to move normally, they require energy and information from the nerves in the body. Nerves secrete chemicals called neurotransmitters. The main neurotransmitter that provides energy to muscles is called acetylcholine. There are receptors on the muscle, which are specifically made for acetylcholine to bind to them. This binding of acetylcholine to the muscle receptor is how muscles receive the energy to move.

Myasthenia gravis (MG) is a disease caused by the inability of acetylcholine to bind to the muscle receptor. If acetylcholine cannot bind to the receptor, then the muscles become weak. In the majority of dogs and cats with myasthenia gravis, the reason that acetylcholine cannot bind to the receptor is because the receptor is already bound to an acetylcholine receptor antibody.
Antibodies are made by the immune system. The immune system should normally function to help protect the body from things like infections, but in animals with myasthenia gravis the immune system becomes over-active and makes antibodies against acetylcholine receptors.
Myasthenia gravis can occur spontaneously due to an abnormally functioning immune system or it can occur secondary to another underlying disease process. Some diseases that can result in myasthenia gravis include cancer, a low thyroid level, and other autoimmune diseases.
What Clinical Signs Occur with Myasthenia Gravis?
Myasthenia gravis causes weakness of muscles, so the most common clinical sign is difficulty walking and needing to rest frequently during exercise. In some animals, all the muscles of the body are affected, but in some cases a single group of muscles is affected (i.e., weakness of just the esophagus muscles, weakness of just the muscles needed for swallowing, and weakness of just the back legs or just the front legs). Cervical ventroflexion is a common symptom of MG in cats.
The esophagus (the tube from the mouth to the stomach) is made up of muscle. Many dogs and cats will develop weakness in the muscles of the esophagus, which causes the esophagus to become enlarged and floppy. This condition is called megaesophagus. When megaesophagus is present, the esophagus cannot move food and water down to the stomach quickly. Megaesophagus leads to regurgitation of the stomach contents and difficulty keeping food and water down.
Dogs and cats with megaesophagus and regurgitation are prone to developing a condition called aspiration pneumonia. Aspiration pneumonia occurs when food, water, or regurgitated fluid accidentally enters the trachea (the tube from the mouth to the lungs) Animals with aspiration pneumonia may develop fever, cough, or difficulty breathing.
Which Animals are Prone to Developing Myasthenia Gravis?
Myasthenia gravis can affect any dog or cat at any age. However, younger (less than 4 years of age) animals and older animals (greater than 9 years of age) develop myasthenia most commonly. Certain breeds of dogs are more commonly affected (like Akitas, terrier breeds, German Shepherd Dogs, German Shorthaired Pointers, Chihuahuas, and Golden Retrievers). Purebred cats are also more commonly affected (like Abyssinians).
What Causes Myasthenia Gravis?
Myasthenia gravis is a classic example of an autoimmune disease. It can occur spontaneously due to an abnormally functioning immune system or it can occur secondary to another underlying disease process. Some diseases that can result in myasthenia gravis include cancer, a low thyroid level, and other autoimmune diseases. In the majority of cases, an underlying cause of myasthenia gravis cannot be identified.
How is Myasthenia Gravis Diagnosed?
The gold standard for a definitive diagnosis of myasthenia gravis is to measure the level of acetylcholine receptor antibodies circulating in the blood stream. This test is called an Acetylcholine Receptor Antibody Titer, and it requires a small blood sample. In a small percentage of dogs and cats with myasthenia gravis, this titer can be normal.
Other tests may be recommended to help support a diagnosis of myasthenia gravis or to help identify an underlying cause of myasthenia gravis. Blood may be drawn for a complete blood count (CBC), chemistry panel, and thyroid level. Chest x-rays are usually recommended to look for megaesophagus, aspiration pneumonia, or a mass in the chest. An abdominal ultrasound may be recommended to look for evidence of cancer in the abdomen.

How is Myasthenia Gravis Treated?
The primary treatment of myasthenia gravis is aimed at making more acetylcholine available to bind to the muscle receptors. If more acetylcholine can bind to the muscle receptors, then the muscles have more available energy and can function normally.
The most common medication that is used to make more acetylcholine available is a drug called Pyridostigmine or Neostigmine. This medication is sometimes referred to as Mestinon or Prostigmin. This medication is given by mouth several times per day. The dose of this medication is usually started at the lower end of the dosing range, and then the dose is slowly increased until the clinical signs of myasthenia gravis are under control. The dosage of this medication is increased slowly because this medication can cause some significant adverse effects. While your pet is on Pyridostigmine or Neostigmine (Mestinon or Prostigmin) you should monitor for adverse effects, and you should alert your veterinarian if these signs occur. These signs include excessive tearing from the eyes, excessive salivation, excessive drooling, vomiting, diarrhea, and a worsening level of muscle weakness.
Since myasthenia gravis is a disorder of the immune system, it is occasionally treated by using medications to help suppress the immune system. This treatment to suppress the immune system may not be necessary in dogs, but it seems to be very helpful in cats. Prednisolone is the most commonly used medication in cats with myasthenia gravis. Prednisolone is a steroid that helps suppress the immune system. Side effects with this medication include an increased appetite, increased thirst, increased urination, and increased restlessness.
Dogs and cats that have megaesophagus may benefit from medications to help decrease the acidity of their stomach contents (antacids). Animals that develop pneumonia will need antibiotics for several weeks, and some pets may require hospitalization to treat their pneumonia.
If your pet has megaesophagus, then the way you feed your pet and what you feed your pet may need to change. It is usually recommended to feed your pet with their head elevated and have your pet remain upright for 15 to 20 minutes after each feeding. The consistency of your pet’s food may also need to change. The ideal consistency is very unique to your pet – some do best with semi-solid food and some do best with solid food. It is a trial-and-error process to determine which consistency of food is right for your pet.

A special chair has been developed to help animals that need to sit upright during feedings, and this chair can be purchased online. It is called a “Bailey Chair,” and these chairs are available at www.baileychairs4dogs.com. This same website also has links to support groups for owners of animals with megaesophagus.
If your dog or cat has severe megaesophagus or regurgitation episodes, then they may benefit from the placement of a feeding tube that bypasses the esophagus. A feeding tube is recommended on a case-by-case basis.
It is important to know that even with appropriate treatment, complete resolution of clinical signs associated with myasthenia gravis may not occur. In most cases the weakness and difficulty walking will resolve with medications. However, megaesophagus can sometimes be very difficult to completely resolve, even with appropriate therapy.
What is the Prognosis for Myasthenia Gravis ?
The prognosis for dogs with myasthenia gravis varies greatly. Approximately 40% of dogs will develop severe enough complications from the disease that their owners elect for humane euthanasia. Dogs with severe megaesophagus and regurgitation and dogs with recurrent episodes of aspiration pneumonia are much more likely to die from the disease. Dogs that do not have megaesophagus, frequent regurgitation, or frequent aspiration pneumonia, tend to do better overall. Interestingly, approximately 88% of dogs in one study had spontaneous remission of their myasthenia gravis within 1 year of treatment. The dogs in that study that did not enter spontaneous remission were the same dogs that had an underlying cause of myasthenia gravis (like cancer).
The prognosis for cats with myasthenia gravis is usually good with treatment. Cats do not develop megaesophagus and aspiration pneumonia as commonly as dogs, which is why cats tend to have a better prognosis. The exact number of cats who enter spontaneous remission is unknown.
Monitoring Recommendations for Dogs and Cats with Myasthenia Gravis:
-
If your pet is receiving Mestinon or Prostigmin (Pyridostigmine or Neostigmine), please contact us if your pet develops excessive tearing from the eyes, excessive salivation or drooling, diarrhea, vomiting, or worsening muscle weakness.
-
Please monitor for signs of aspiration pneumonia, especially if your pet has megaesophagus. Common signs of pneumonia include a new or worsening cough, difficultly breathing, pale/gray/blue gums, lethargy or decreased activity level, and decreased appetite. Please contact us or your veterinarian if these signs occur.
-
Please contact us if episodes of regurgitation worsen or do not improve. Also, please let us know if you feel that your pet is losing weight.
References
- Dickinson PJ, Sturges BK, Shelton GD, et al. Congenital Myasthenia Gravis in Smooth-Haired Miniature
- Dachshund Dogs. J Vet Intern Med 2005;19:920-923.
- Meola SD, Mazzaferro EM, Wheeler JL, et al. Medical and surgical management of severe barium
aspiration in a dog. J Vet Emerg Crit Care 2008;18(6):639-645. - Dewey CW, Bailey CS, Shelton GD, et al. Clinical forms of acquired myasthenia gravis in dogs: 25cases
(1988-1995), J Vet Intern Med 1997;11:50-57. - Ducote JM, Dewey CW, Coates JR. Clinical forms of acquired myasthenia gravis in cats. Compend
Contin Educ Pract Vet 1999;21:440-448. - Dewey CW. Junctionopathies: Disorders of the Neuromuscular Junction. A Practical Guide to Canine
and Feline Neurology, 2008:517-536. - Shelton GD, Lindstrom JM. Spontaneous remission in canine myasthenia gravis: implications for
assessing human MG therapies. Neurology 2001 Dec 11; 57(11):2139-41. - Dewey CW, Coates JR, Ducote JM, et al. Azathioprine therapy for acquired myasthenia gravis. JAAHA 1999; 35(5):396-402.
- Bexfield NH, Watson PJ, Herrtage ME. Management of myasthenia gravis using cyclosporine in 2 dogs. JVIM 2006; 20(6):1487-90.
- Foy DS, Trepanier LA, Shelton GD. Cholinergic crisis after neostigmine administration in a dog with acquire focal myasthenia gravis. JVECC 2011; 21(5):547-551.
- Gajanayake I, Niessen JM, Cherubini GB, et al. Autoimmune myasthenia gravis and dysautonomia in a dog. JSAP 2008; 49:593-595.
- Dewey CW, Cerda-Gonzalez S, Fletcher DJ, et al. Mycophenolate mofetil treatment in dogs with serologically diagnosed acquired myasthenia gravis: 27 cases (1999-2008). JAVMA 2010; 236:664-668.
- Abelson AL, Shelton GD, Whelan MF, et al. Use of mycophenolate mofetil as a rescue agent in the treatment of severe generalized myasthenia gravis in three dogs. JVECC 2009; 19(4):369-374.
- Whitley NT, Day MJ. Immunomodulatory drugs and their application to the management of canine immune-mediated disease. JSAP 2011; 52:70-85.
- Spurlock NK, Prittie JE. A review of current indications, adverse effects, and administration recommendations for intravenous immunoglobulin. JVECC 2011; 21(5):471-483.
- Bartges JW, Klausner JS, Bostwick EF, et al. Clinical remission following plasmapheresis and corticosteroid treatment in a dog with myasthenia gravis. JAVMA 1990; 196(8):1276-1278.
- Galin FS, Chrisman CL, Cook JR, et al. Possible therapeutic vaccines for canine myasthenia gravis: Implications for the human disease and associated fatigue. Brain, Behavior, and Immunity 2007; 21(323-331).
- Rutter, CR, et al. Outcome and medical management in dogs with LMN disease undergoing mechanical ventilation: 14 cases (2003-2009). JVECC 2011; 21(5):531-541.
- Kent M, Glass EN, Acierno M, et al. Adult onset acquired myasthenia gravis in three great Dane littermates. JSAP 2008; 49:647-650.
- Shelton GD, Schule A, Kass PH. Risk factors for acquired myasthenia gravis in dogs: 1,154 cases (1991- 1995). JAVMA 1997; 2111(11):1428-1431.
- Shelton GD. Myasthenia gravis and disorders of neuromuscular
